
Tumor-destroying soundwaves receive FDA approval for liver treatment in humans
Technique developed at the University of Michigan provides a non-invasive alternative to surgery, chemotherapy and radiation treatments for cancer.

Technique developed at the University of Michigan provides a non-invasive alternative to surgery, chemotherapy and radiation treatments for cancer.
BY: JIM LYNCH
The U.S. Food and Drug Administration has approved the use of sound waves to break down tumors—a technique called histotripsy—in humans for liver treatment.
Pioneered at the University of Michigan, histotripsy offers a promising alternative to cancer treatments such as surgery, radiation and chemotherapy, which often have significant side effects. Today, Food and Drug Administration’s (FDA) officials awarded clearance to HistoSonics, a company co-founded in 2009 by U-M engineers and doctors for the use of histotripsy to destroy targeted liver tissue.
A human trial underway since 2021 at the U-M Rogel Cancer Center and other locations has treated patients with primary and metastatic liver tumors via histotripsy, demonstrating the technology’s ability to meet the testing’s primary effectiveness and safety targets.
“Histotripsy is an exciting new technology that, although it is in early stages of clinical use, may provide a non-invasive treatment option for patients with liver cancer. Hopefully it can be combined with systemic therapies for a synergistic therapeutic effect,” said Mishal Mendiratta-Lala, an assistant professor of radiology with Michigan Medicine and principal investigator on the trial at U-M.
HistoSonics can now market and sell its histotripsy delivery platform, called Edison, to hospitals and medical professionals for use in liver treatments. The company is headquartered in Minneapolis, while its advanced research and development is located in Ann Arbor.

Dr. Ryan Miller, Ph.D., Manager of Advanced Systems at HistoSonics, adjusts the transducer head on the Edison Platform as he observes a histotripsy treatment plan at HistoSonics in Ann Arbor. Photo: Erica Bass/Michigan Medicine
Histotripsy works by using targeted ultrasound waves to form microbubbles within the tumor. The forces created as those bubbles form and collapse cause the mass to break apart, killing tumor cells and leaving the debris to be cleaned up by the immune system.
What that could mean for patients is treatment without the physical toll of radiation or chemotherapy, fewer concerns with drug compatibility, far shorter recovery times than with surgery and less treatment discomfort.
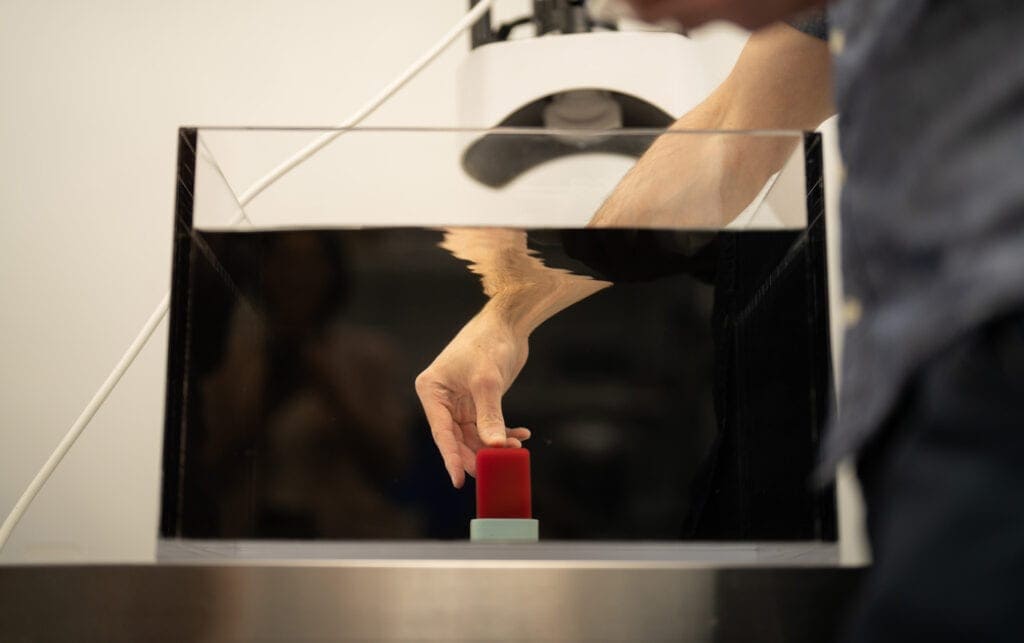
Dr. Alex Duryea, Ph.D., Manager of Applied Research at HistoSonics, adjusts an ultrasound “phantom”—a gel mixed with red blood cells that serves as the test’s tumor—prior to performing a histotripsy treatment demonstration at HistoSonics. Photo: Erica Bass/Michigan Medicine
This is possible because it is much easier to ensure that histotripsy treatments are hitting the tumor, and not healthy tissue, compared to radiation or invasive procedures. Histotripsy relies on focusing acoustic waves of high energy ultrasound to concentrate the energy enough to form bubbles, and the Edison machine can make sure that region is confined to the tumor. In contrast, radiation affects everything in its path through the body.
In addition, the histotripsy system has onboard diagnostic ultrasound imaging, the kind used to see babies in the womb. It is used to plan and observe the treatment in real time. Physicians have a live view of the “bubble cloud” and how tissue is responding to the therapy.
And histotripsy’s potential benefits go beyond tumor destruction. In the last year, a pair of pre-clinical studies in rodents suggest that in the clean-up process, the immune system learns how to identify cancer cells as threats. This can enable the body to continue fighting the initial tumor and help activate a natural immune response to the cancer.
In the first study, even after destroying only 50% to 75% of the liver tumor volume by histotripsy, the rats’ immune systems were able to clear away the rest, with no evidence of recurrence or metastases in more than 80% of animals.
Earlier this year, a second study showed that histotripsy breaks down the cancer cell wall’s “cloak”—revealing proteins that the immune system can use to identify threats, known as antigens. These antigens are removed during surgery or destroyed during chemotherapy and radiation. By instead destroying a cancer cell’s outer wall, histotripsy lays bare the tumor antigens for the immune system to identify and use for targeted attacks on other cancer cells.

“We want to leverage histotripsy’s immuno stimulation effects and hopefully combine them with immunotherapy or drug delivery,” said Zhen Xu, a U-M professor of biomedical engineering, an inventor of the histotripsy approach and a co-founder of HistoSonics. “That will move histotripsy from a local therapy into one that can treat tumors globally all over the body and eventually into a cure. In terms of the cancer treatment, that will be the next step, and I feel very excited about the potential.”
Mendiratta-Lala, Xu and the University of Michigan have a financial interest in HistoSonics. The company was formed with support from U-M’s Coulter Translational Research Program and Innovation Partnerships, U-M’s hub for research commercialization.
RELATED LINKS