
Nanoparticles reprogram mouse immune systems to cope with allergens
Treatment suppressed anaphylaxis and reduced gut inflammation after just two intravenous infusions.

Treatment suppressed anaphylaxis and reduced gut inflammation after just two intravenous infusions.
By Patricia DeLacey, Michigan Engineering
Two doses of allergen-encapsulating nanoparticles delivered intravenously prevented anaphylaxis during a food allergy test in mice, according to a study led by University of Michigan researchers.
The results, published in Advanced Healthcare Materials, offer a potential path to improving the ease of allergy immunotherapies in humans which currently require daily doses of the allergen.
In addition to the research in mice, this allergen-encapsulating nanoparticle platform has completed a phase two clinical trial for treating the autoimmune condition celiac disease.
Food allergies form when a person’s immune system misidentifies a harmless food protein—the allergen—as a threat. The immune system behaves similarly to how it would identify a virus, harmful bacteria or toxin, and mounts a defensive response to fight off the threat.
“It is not clear why certain individuals develop food allergies, and current treatments remain very limited”, said Jessica O’Konek, a research assistant professor at the Mary H. Weiser Food Allergy Center at Michigan Medicine and co-corresponding author on the study.
While clinical management often focuses on allergen avoidance, patients are left susceptible to accidental exposures, which could be life-threatening. In the U.S., 51% of adults and 42% of children with a food allergy reported an incidence of a severe allergic reaction where anaphylaxis, low blood pressure, trouble breathing or wheezing occurred, sometimes leading to emergency room visits.
Allergen-specific immunotherapies aim to treat food allergies with a daily dose of the food allergen. Over time, patients can become desensitized, yet the allergic response may re-emerge after patients stop taking the allergen daily.
“Rather than focusing on desensitization, treatment with allergen-encapsulating nanoparticles actually retrains the immune system not to react to an allergen—a process termed tolerance,” said Lonnie Shea, a Steven A. Goldstein Collegiate Professor of Biomedical Engineering at U-M and co-corresponding author on the study.
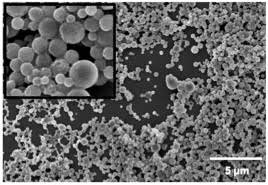
At just 500 nanometers in diameter, these particles are 0.5% the width of a human hair and hold a negative surface charge that targets them to immune cells.
“These characteristics of the nanoparticle make them appear like debris from dying cells, which are generally not viewed as dangerous. The encapsulated allergen is processed by the immune cells without upregulating danger signals that would normally activate an immune response,” said Shea.
Once taken up, these nanoparticles interact with immune system pathways to suppress T helper 2 cells, an immune cell type that causes inflammation in response to allergens. The treatment even reprograms some inflammatory T helper 2 cells to become regulatory T-cells, a cell type that regulates your immune system not to attack your own cells, which lessens the body’s reaction to the allergen.
The researchers used a mouse model of an egg allergy where they first sensitized mice to ovalbumin, an allergy-inducing protein in egg whites, then treated mice with either a placebo or ovalbumin-encapsulating nanoparticles dissolved in a phosphate-buffered saline.
The mice then underwent an oral food challenge, a common diagnostic for food allergies where a patient eats suspected allergen to determine if anaphylaxis occurs.
Mice treated with ovalbumin nanoparticles did not have an anaphylactic response that was observed in the control condition and had less food allergy reactions overall, including diarrhea.
Tissue and blood samples collected from these mice helped unravel the cellular pathways and found that treatment reduced basophil and mast cell frequency in the gut, indicating less allergic inflammation.
Studies are currently investigating how long these nanoparticles prevent a reaction to the allergen.
“Because food allergies trigger the same T helper cell response, this platform could be modified to encapsulate and deliver any allergen to enable tolerance in just a few doses,” said Shea.
Shea is also a professor of chemical engineering and surgery.
O’Konek is also a William Chandler Swink Research Professor and a research assistant professor in the Michigan Nanotechnology Institute for Medicine and Biological Sciences and Michigan Medicine Department of Internal Medicine.
Joel Whitfield in the Rogel Cancer Center Immunology Core performed the ELISAs.
This work was supported by the National Institute of Allergy and Infectious Diseases (R01 AI155678).
Additional co-authors: Michael N. Saunders, Laila M. Rad, Laura A. Williams, Russell R. Urie, Sarah E. Hocevar, Amogh R. Angadi, Elizabeth J. Bealer, Kelly Crumley, Kate V. Griffin, and Brian C. Ross of the University of Michigan Department of Biomedical Engineering; Jeffrey J. Landers, Katarzyna W. Janczak, and Olivia E. Benson of the University of Michigan Mary H. Weiser Food Allergy Center; Miguel Quiros, Charles A. Parkos, and Asma Nusrat of the Michigan Medicine Department of Pathology; and Ming-Yi Chiang, Stephen D. Miller, and Joseph R. Podojil of the Northwestern University Department of Microbiology-Immunology.
Full citation: “Allergen-encapsulating nanoparticles reprogram pathogenic allergen-specific Th2 cells to suppress food allergy,” Michael N. Saunders, Laila M. Rad, Laura A. Williams, Jeffrey J. Landers, Russell R. Urie, Sarah E. Hocevar, Miguel Quiros, Ming-Yi Chiang, Amogh R. Angadi, Katarzyna W. Janczak, Elizabeth J. Bealer, Kelly Crumley, Olivia E. Benson, Kate V. Griffin, Brian C. Ross, Charles A. Parkos, Asma Nusrat, Stephen D. Miller, Joseph R. Podojil, Jessica J. O’Konek, and Lonnie D. Shea, Advanced Healthcare Materials (2024). DOI: 10.1002/adhm.202400237