One Lab, Three Approaches to Restoring Ovarian Function
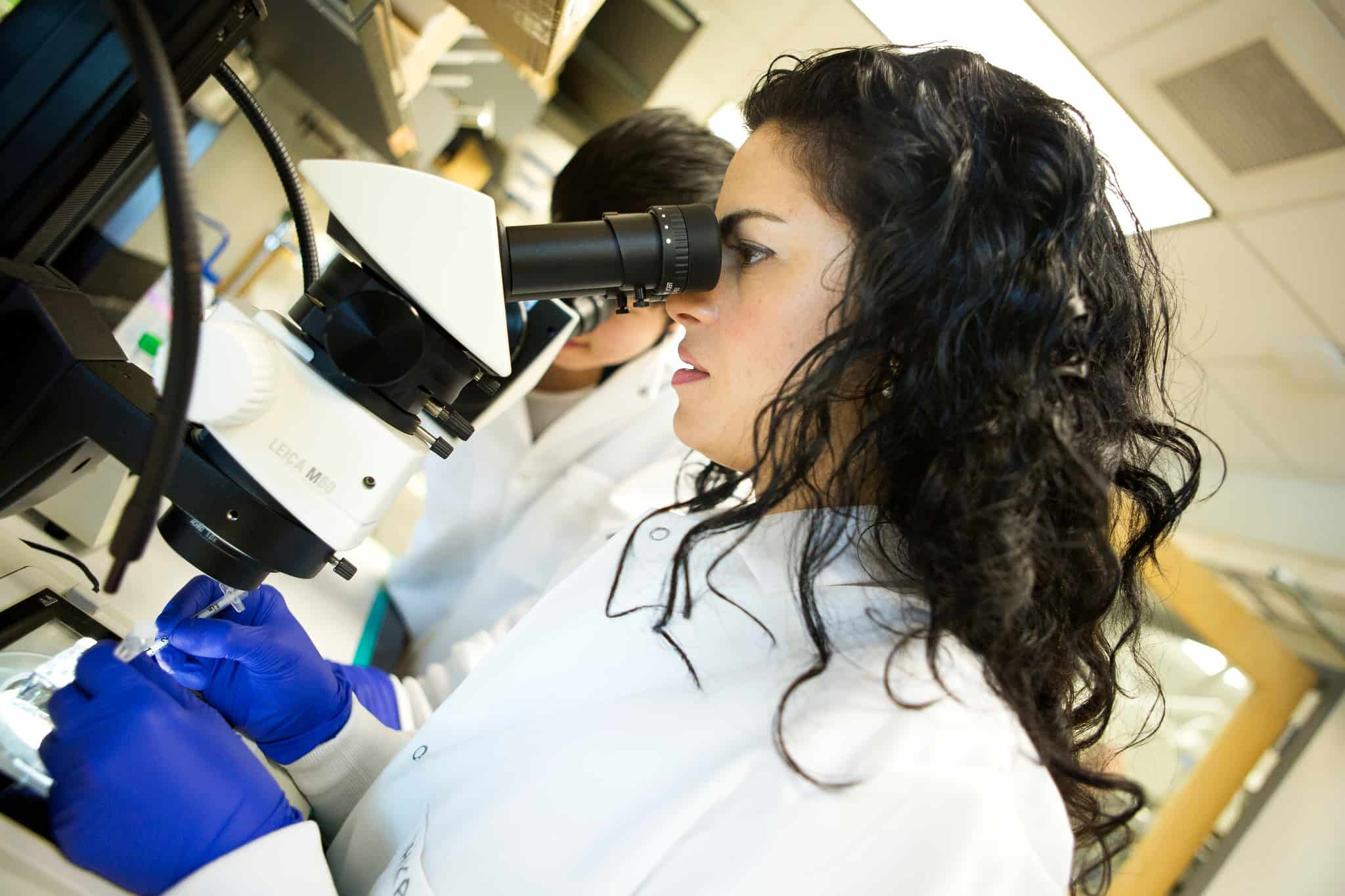
Shikanov’s first project aims to restore endocrine function in girls with damaged ovaries, allowing them to undergo physiologic puberty.
Shikanov’s first project aims to restore endocrine function in girls with damaged ovaries, allowing them to undergo physiologic puberty.
By Aimee Balfe
BME Assistant Professor Ariella Shikanov has just received an NSF CAREER award to help fund one of the three approaches her lab is taking to help restore ovarian function in women and girls undergoing treatment for cancer and autoimmune disease that is toxic to the ovaries.
While physicians can freeze a woman’s eggs, allowing her to later have a biologically related child, the process isn’t suitable for some patients, including young girls. It also doesn’t address the issue of ovaries’ endocrine function. “Ovaries are not only about making babies,” says Shikanov, “they also produce estrogen, progesterone, and other hormones that are very important for the health of a woman’s bones, cardiovascular system, and skin.”
“OVARIES ARE NOT ONLY ABOUT MAKING BABIES…THEY ALSO PRODUCE ESTROGEN, PROGESTERONE, AND OTHER HORMONES THAT ARE VERY IMPORTANT FOR THE HEALTH OF A WOMAN’S BONES, CARDIOVASCULAR SYSTEM, AND SKIN.” Shikanov
They’re also essential for enabling girls to go through puberty. Girls who’ve lost ovarian function require synthetic hormones, whose long-term use carries a health risk. In addition, the dosage has to be just right. Too little and the girls won’t grow sufficiently. Too much and the bones’ growth plates close prematurely. Without optimal dosing, the girls are at increased risk for various bone, cardiovascular, and metabolic problems like diabetes and obesity.

Shikanov would become captivated by this issue and begin down a road that would lead her from the Hebrew University in Jerusalem to U-M via a postdoctoral fellowship in the lab of Lonnie Shea. Then at Northwestern, and now U-M’s William and Valerie Hall Chair and Professor of BME, Shea had been working on ovarian tissue engineering and needed a postdoc with expertise in polymer synthesis and hydrogel development. Shikanov, a medicinal chemist by training, had the right skill set.
“He told me, ‘Don’t worry; you’ll learn about reproduction,’” she says. Over the next four years, she found herself doing surgeries in mice, looking for ways to make ovarian tissue transplantation more successful, and developing synthetic culture environments for ovarian follicles – the structures that contain immature eggs and are essential to endocrine function.
The latter offered an intriguing engineering challenge. “We had to design a hydrogel that would be soft enough not to kill an ovarian follicle, but rigid enough to support its 3D structure as it matures and expands 100 times in volume,” she says. “It also had to be physiologic, allowing the diffusion of nutrients and oxygen.”
“WE HAD TO DESIGN A HYDROGEL THAT WOULD BE SOFT ENOUGH NOT TO KILL AN OVARIAN FOLLICLE, BUT RIGID ENOUGH TO SUPPORT ITS 3D STRUCTURE AS IT MATURES AND EXPANDS 100 TIMES IN VOLUME” Shikanov
She was deep in this work when U-M announced a cluster-hire position in reproductive biomaterials that precisely matched her expertise. She was hired in 2012, launching a lab that would address ovarian function through three distinct but mutually reinforcing projects.
Restoring endocrine function in girls
Shikanov’s first project aims to restore endocrine function in girls with damaged ovaries, allowing them to undergo physiologic puberty. She is developing an implant that encapsulates donor ovarian tissue in an immunoisolating hydrogel. Injected under the skin, it won’t restore fertility but would stimulate the production of estrogen at this critical time.
“Puberty starts in the brain,” says Shikanov. “The hypothalamus secretes a hormone, which stimulates the pituitary gland to secrete follicular stimulating hormone, which tells the ovarian tissue to secrete estrogen. Then the estrogen goes back to the brain, controlling things through a finely tuned loop. This is what allows us to go through puberty, and this why it is so important to have a healthy and functioning ovarian tissue that we aim to engineer.”
With a grant from The Hartwell Foundation, her lab has already demonstrated in mice that the process works and that its longevity is determined by the number of follicles implanted. She plans to move to larger animal models before testing the product in humans.
Understanding how ovarian follicles develop
Shikanov’s second project, for which she won her CAREER award, aims to understand the cell signaling involved in the development of ovarian follicles so she can design better culture systems for harvested tissue.
Harvesting of immature ovarian follicles holds promise for restoring fertility when a woman can’t freeze her eggs – either because she doesn’t have time to undergo ovarian stimulation prior to starting treatment or because she has a hormone-driven cancer where stimulation would be inappropriate. The problem has been getting follicles to survive and mature in culture.
The reason for this, says Shikanov, is that follicles’ essential signaling networks are poorly understood. “Right now, we know that follicles grow best when they’re co-cultured with other follicles and stem cells, but we don’t know why.”
She hopes to remedy this through mechanistic studies of folliculogenesis. Using transcription factor reporters, metabolomics, and systems biology, she aims to reveal the identity, timing and activity pattern of secreted growth factors and transcription factors that allow follicles to grow.
During the project, she plans to continue collaborating with Lonnie Shea, as well as with BME computational modeling expert David Sept, new faculty member Kelly Arnold, and U-M’s metabolomics core, MRC2.
She will start the experimental work in mice, but hopes to move to human tissue in a matter of years. “I want to get to the point where I can take one follicle and say, if I add this list of factors at these concentrations in this timing sequence, I will be able to grow the follicle without adding other follicles or cells,” she says.

Designing an artificial ovary
Her final project is the design of an artificial ovary. This involves encapsulating the smallest, primordial follicles in a synthetic polymer that mimics the ovaries’ natural environment with the goal of restoring both fertility and endocrine function. She expects that her mechanistic studies will offer substantial insights to this work.
Shikanov says her research is extremely gratifying, and she enjoys introducing it to young people, especially women, through camps and programs for middle and high schoolers. In addition, her lab is always seeking talented postdocs interested in learning more about biomaterials in reproductive sciences. She can be contacted at [email protected].