A team of U-M researchers, led by Aaron Morris, Assistant Professor, Biomedical Engineering, recently received a Lupus Innovation Award (LIA) from the Lupus Research Alliance. The LIA, a grant of up to $450,000 for three years, provides early-stage support for highly innovative approaches to addressing major challenges in lupus research.
Dr. Morris is working with J. Michelle Kahlenberg, M.D., Ph.D., a rheumatologist at Michigan Medicine; Celine Bertheir, Ph.D., an associate research scientist in the Michigan Kidney Translational Medicine Center, Internal Medicine, at Michigan Medicine; and Jeffrey Hodgin, M.D., Ph.D., an associate professor of pathology and investigative renal pathologist. The team’s goal is to examine novel ways that might be useful in assessing if a patient is developing lupus nephritis.
“My lab studies autoimmune disease, and we mostly have focused on multiple sclerosis, an autoimmune disease that affects the central nervous system,” said Dr. Morris, “but I was interested in thinking about autoimmunity more generally and what we might be able to do to help other autoimmune conditions.”
Dr. Morris had heard about the work that Dr. Kahlenberg is conducting in lupus research. “She’s a physician scientist and treats patients who have lupus,” Dr. Morris said. “Dr. Kahlenberg also runs a lab that studies the basic mechanisms of the disease. I told her about some of the work we had done in multiple sclerosis, and said that maybe we could collaboratively apply our resources in lupus research.”
Lupus, also known as systemic lupus erythematosus (SLE), is a complicated disease that can affect different organ systems. The most common symptom is a “butterfly” rash, which is a very distinctive rash people often get. Sometimes this leads to a quick diagnosis. However, not every lupus patient experiences these rashes.
“Even in people who get the rashes, there are other parts of the disease that can be hard to diagnose,” Dr. Morris said. “Lupus nephritis is the autoimmunity affecting the kidneys, and that can be really challenging to monitor. Unfortunately, patients who develop lupus are at risk for lupus nephritis. Right now, the medical community doesn’t have a quick way to determine who will ultimately get it. About 5 million people worldwide have lupus, and lupus nephritis develops in almost half of those patients. The question is not only will it develop, but when will it develop and what to do about it.”
Currently, physicians monitor kidney function with urine tests. “Unfortunately, often by the time we can tell that kidney function is compromised, the damage is done,” said Dr. Morris. “We would prefer to know sooner.” Some doctors perform ongoing kidney biopsies to monitor kidney function, but this can be an invasive, uncomfortable procedure that can expose a patient to possible risks and complications.
Dr. Morris’ team will focus on identifying a new diagnostic tool for monitoring lupus, specifically lupus nephritis.
The team will use flow cytometry and RNA sequencing to examine how cell populations and their gene expression are changing in the implants in disease and whether that correlates with other tissues. The researchers will then conduct a more detailed analysis of single-cell sequencing of the implants in kidneys and other organs. “What we hope we can find are changes that are specific to lupus nephritis,” Dr. Morris said.
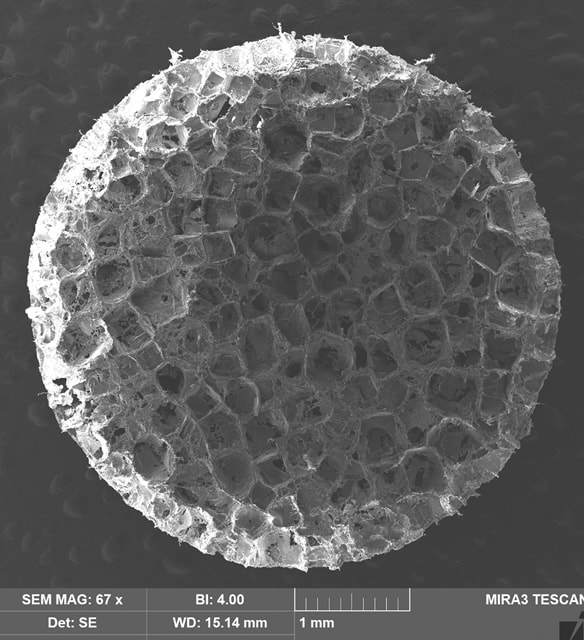
The device that will be implanted is a small cylinder, 5 mm in diameter and 2 mm tall. It is made of an FDA-approved polymer, is very porous and looks a lot like a sponge. “We will take a biopsy of the cells that are collected in this site after about 3 to 6 weeks to determine their changes.”
The second part of the study is focused on treatment and trying to manage the response to treatment. “We’re going to test whether the implants that can be useful in monitoring disease can also help monitor responses to therapy. We will test a couple of different treatments for lupus and track if the implant can monitor the efficacy of the therapeutics in preventing lupus nephritis.”
Dr. Morris said that U-M provides an excellent location to conduct this research. “I’m really excited about the project and I am confident we have a good team for this,” he said. “I’m excited at the opportunity that we might be able to take this platform and make a real difference in lupus because it is an understudied disease that affects many people.”