Surgeon uses academic development time to collaborate with Biomedical Engineering
Collaboration serves to inform the need for surgical interventions
Collaboration serves to inform the need for surgical interventions
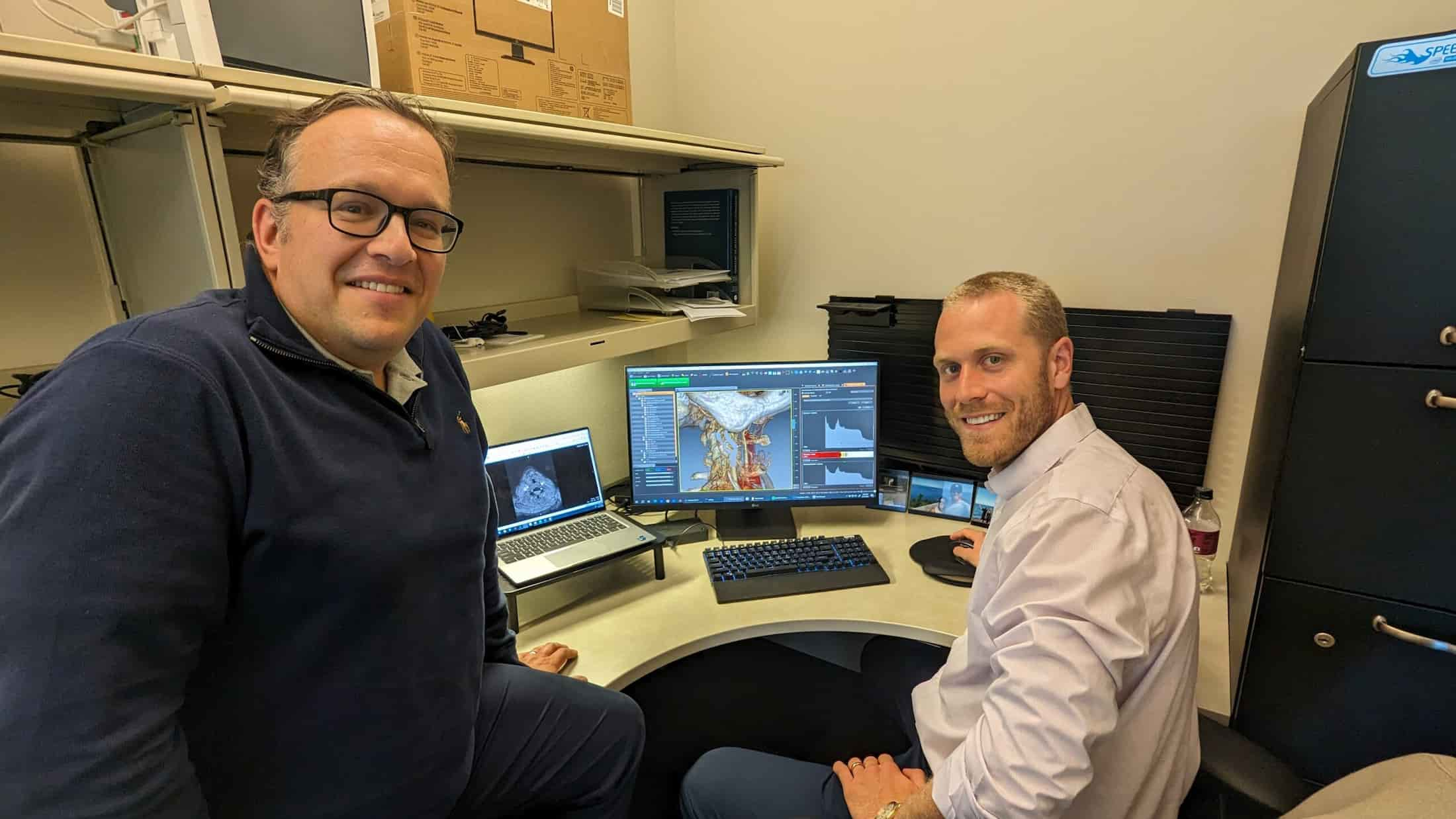
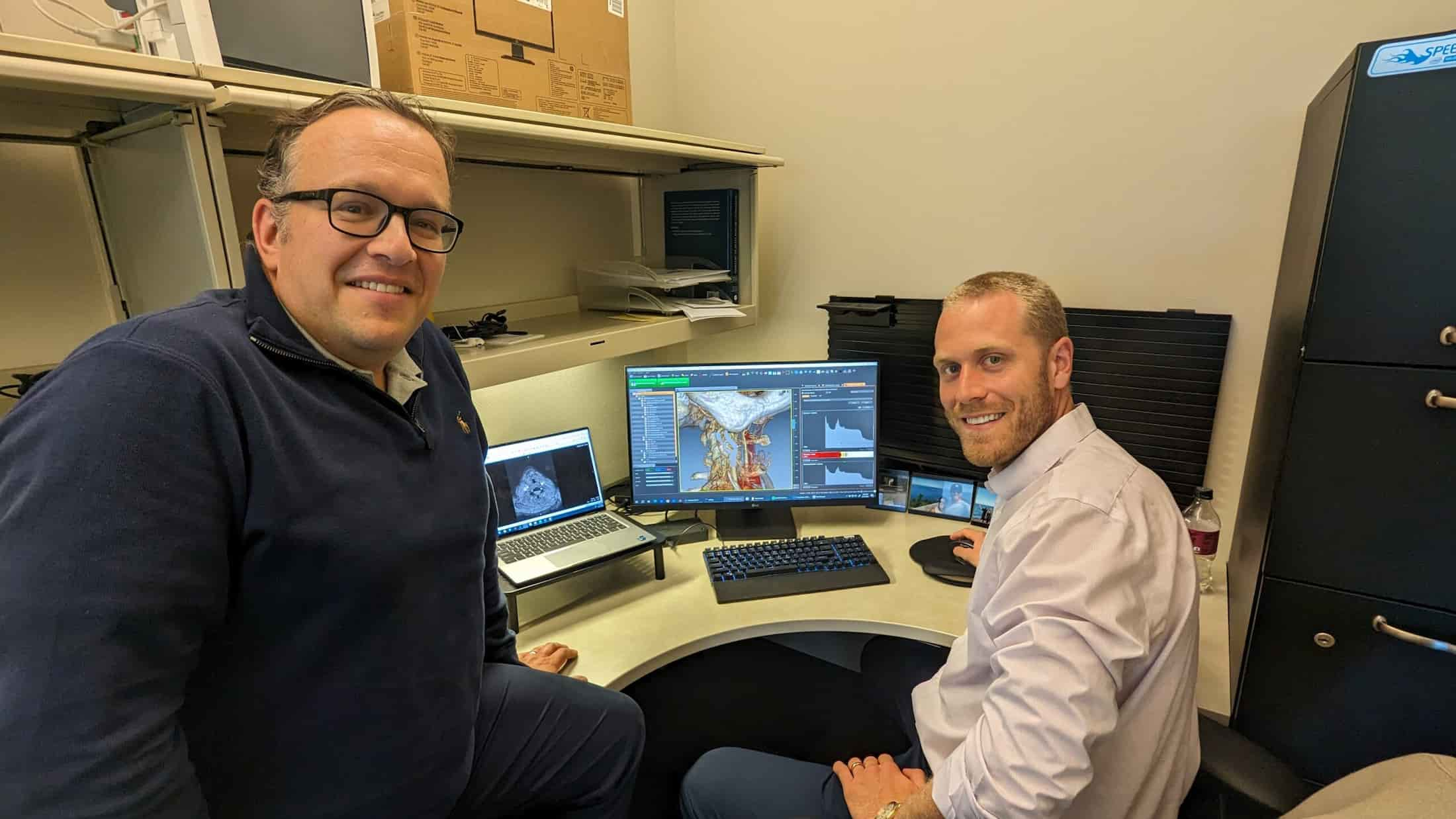
Drew Braet is a fourth-year resident in Vascular Surgery and is taking his two-year academic development time to work with C. Alberto Figueroa, the Edward B Diethrich M.D. Research Professor of Biomedical Engineering and Vascular Surgery, professor of surgery, Medical School and professor of biomedical engineering, Medical School and College of Engineering. Dr. Braet’s goal from this collaboration is to gain a better understanding of determining which patients are most likely to benefit from surgical intervention.
“I sought to work with Biomedical Engineering, and Dr. Figueroa, specifically, by choice,” Dr. Braet said. “Early in my training, I became frustrated with the lack of information we often have about vascular disease, particularly when looking at which patients we should or should not offer surgery to. It’s pretty typical in medicine that things aren’t black and white, and that there are many gray areas. We’re really lacking clear data in a lot of different realms that can help us with decision making.”
“It is not typical that a surgeon would do research in an engineering laboratory like ours,” said Dr. Figueroa. “To have someone who goes from operating on patients to then spending two years learning analytical tools–imaging tools, modeling tools and computational tools–is somewhat unique.” A two-year research period is mandatory at U-M, but most people in the training program do not end up focusing on Engineering. “Historically, most trainees do time working in a basic science wet laboratory,” he added.
Dr. Braet was researching information in his quest to learn more ways data analysis can inform surgical interventions, and through a Google search, came upon Dr. Figueroa’s lab.
“I thought what he was doing in using computational methods in advanced imaging analysis would really help me,” Dr. Braet said. “I wanted to learn a tool set to be able to explore some of the questions I had. I ultimately want to improve our understanding and to provide better patient care. We met early on in my intern year. I heard about some of the work they were doing in the lab and explained some of the things I was interested in. In my intern year, we started doing a smaller project. Dr. Nick Burris, a radiologist, and I worked on that for a year, and we were able to publish a paper. From there, we started thinking about a bigger project that we could do during my dedicated time, and that led us to do my current project and current NIH F32 fellowship, where I’m looking at patients with high-grade asymptomatic carotid artery disease.”
The carotid artery is the artery in your neck that goes to your brain. “Patients who have narrowings in that artery have buildup of cholesterol plaque, the same kind of plaque that can lead to heart attacks,” Dr. Braet said. “That plaque can break off, and cause a stroke. The way that we think about these plaques in medicine is based on historical studies which suggest that the percentage of narrowing of the carotid artery is related to the risk of having a stroke. When I think about that from a biophysical and biomechanical standpoint, it doesn’t make sense. Not to discredit the studies that were previously done, this is what science has shown and we have helped a lot of people by thinking that way. But when you really boil it down to the biophysics of blood flow, that doesn’t make sense, because plaques rupture when the forces exerted on them exceed the strength of the tissue. We’re doing a computational modeling study by looking at the pressure differences, the velocity differences and the wall shear stress on carotid artery plaques to try to get a better understanding of the hemodynamic strains and stresses of the plaque and thus the risk of stroke. This could potentially lead to an entirely new way of looking at the way patients present with this particular issue. In a perfect world, 20 years from now, it would be great if the medical field could be using some of the things that we’re studying today. These kinds of engineering, imaging and modeling analyses, I think, will help us do a much better job with risk stratification that ultimately will determine whether to perform surgery or to watch a patient more conservatively.”
Dr. Braet noted that it is “refreshing” to learn to examine problems in a different way. ”In the big picture, if more surgeons and more doctors learned to look at challenges differently, we might be able to be more creative in the treatments that we can offer,” Dr. Braet said. The analysis of big data and the use of technological innovations are playing increasingly important roles in medicine, and Dr. Braet wants to understand how Engineering can assist the profession.
Dr. Figueroa noted the value of this type of mentorship for the mentor as well as the mentee. “It’s interesting because someone like Drew has a very different background and very different ways of seeing a problem than someone from a traditional engineering background,” he said. “Everybody talks about translation and reaching out, and when you are in engineering, you want to have your tools applied, but it’s actually quite difficult to do because of how distant the training and the day-to-day professional thought processes these two groups have. In engineering, you typically say you want to talk to clinicians because at the end, they are your customers for developing a new device or a new diagnostic procedure. Eventually, they’re going to have to use it and understand it, right?”
The fact that the University of Michigan has a Biomedical Engineering Department that is jointly in both the Medical School and in the College of Engineering enhances these opportunities for collaboration. There are a lot of institutions out there where perhaps they have a biomedical engineering department, but they don’t have a medical school,” Dr. Figueroa said. “In those institutions, this understanding is much harder to achieve because the engineering folks are kind of isolated and they don’t have ready access to clinical peers.”
Dr. Figueroa added that the opportunity to serve as a mentor is a rewarding experience, professionally and personally. “To me, it’s important that when I one day finish my career, I will have contributed to training a small group of clinicians who have an engineering thought process,” he said.