Tumors partially destroyed with sound don’t come back, in rats
Technique pioneered at the University of Michigan could improve outcomes for cancer and neurological conditions.
Technique pioneered at the University of Michigan could improve outcomes for cancer and neurological conditions.
Non-invasive sound technology developed at the University of Michigan breaks down liver tumors in rats, kills cancer cells and spurs the immune system to prevent further spread—an advance that could lead to improved cancer outcomes in humans. By destroying only 50% to 75% percent of liver tumor volume, the rats’ immune systems were able to clear away the rest, with no evidence of recurrence or metastases in more than 80% of animals.
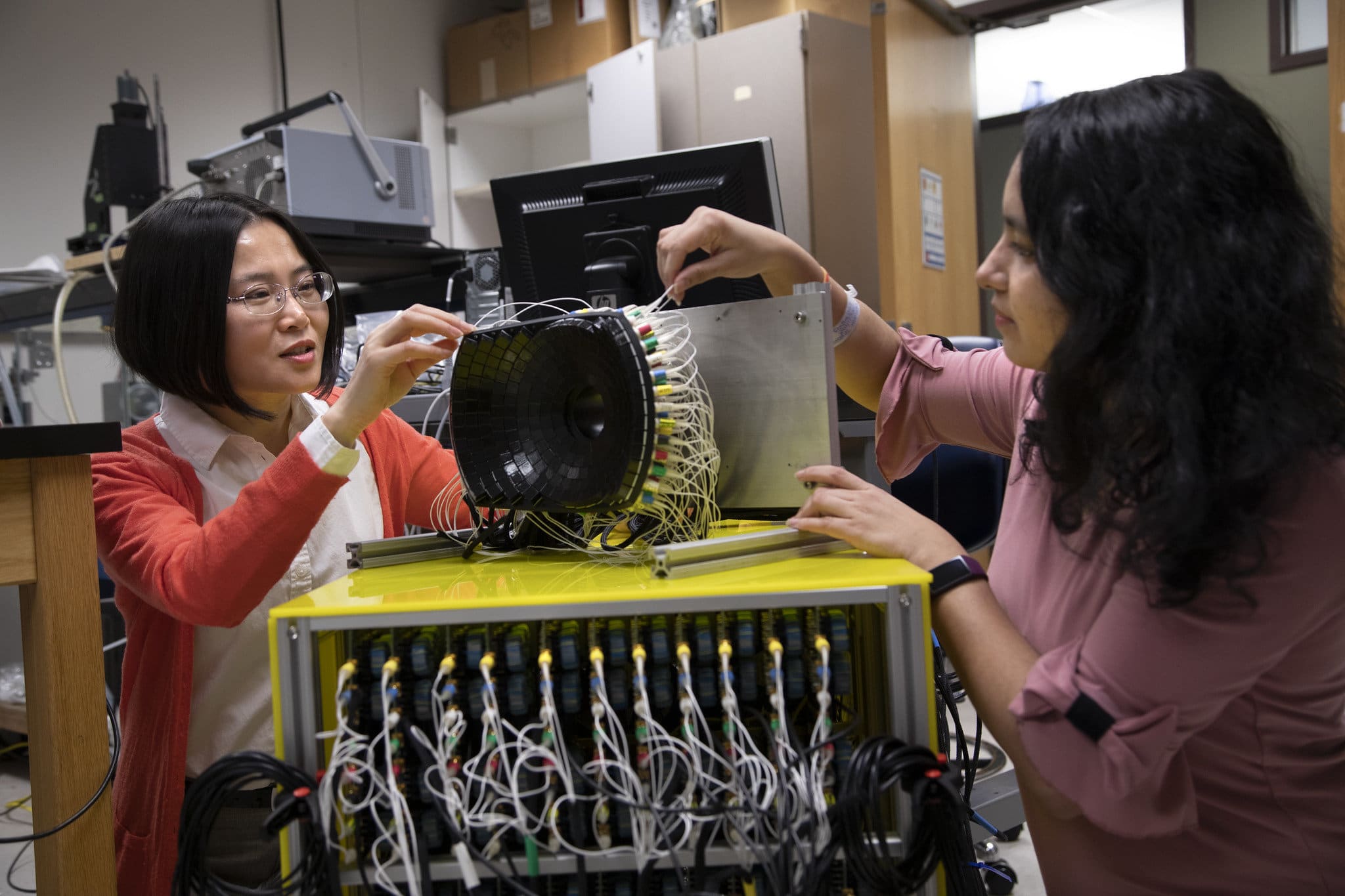
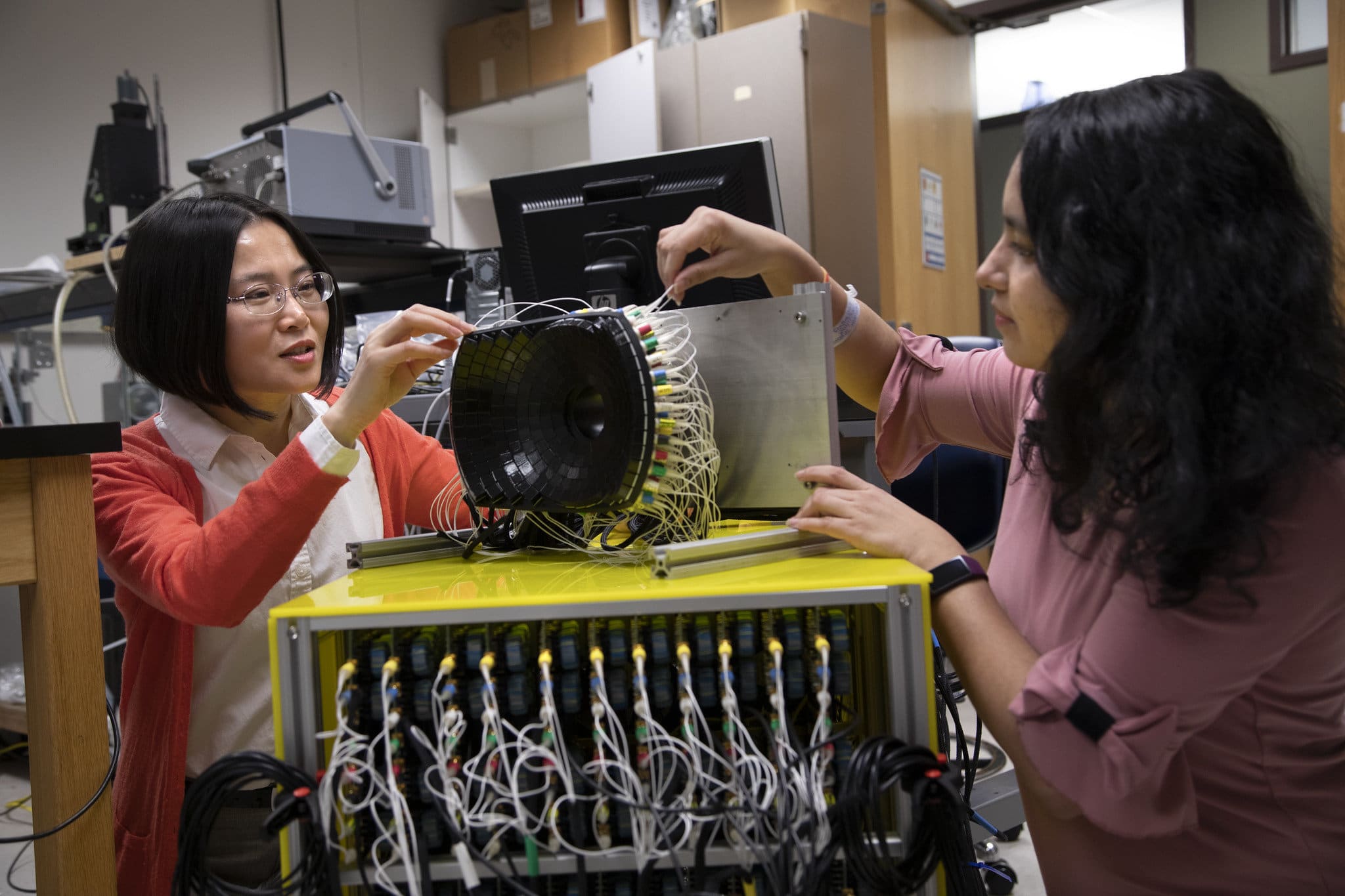
“Even if we don’t target the entire tumor, we can still cause the tumor to regress and also reduce the risk of future metastasis,” said Zhen Xu, a professor of biomedical engineering at U-M and corresponding author of the paper in Cancers.
Results also showed the treatment stimulated the rats’ immune responses, possibly contributing to the eventual regression of the untargeted portion of the tumor and preventing further spread of the cancer.
The treatment, called histotripsy, non-invasively focuses ultrasound waves to mechanically destroy target tissue with millimeter precision. The relatively new technique is currently being used in a human liver cancer trial in the US and Europe.
In many clinical situations, the entirety of a cancerous tumor cannot be targeted directly in treatments for reasons that include the mass’ size, location or stage. To investigate the effects of partially destroying tumors with sound, this latest study targeted only a portion of each mass, leaving behind a viable intact tumor. It also allowed the team, including researchers at Michigan Medicine and the Ann Arbor VA Hospital, to show the approach’s effectiveness under less than optimal conditions.
“Histotripsy is a promising option that can overcome the limitations of currently available ablation modalities and provide safe and effective non-invasive liver tumor ablation,” said Tejaswi Worlikar, a PhD student in biomedical engineering. “We hope that our learnings from this study will motivate future pre-clinical and clinical histotripsy investigations towards the ultimate goal of clinical adoption of histotripsy treatment for liver cancer patients.”
Liver cancer ranks among the top ten causes of cancer related deaths worldwide and in the United States. Even with multiple treatment options, the prognosis remains poor with five-year survival rates less than 18% in the US. The high prevalence of tumor recurrence and metastasis after initial treatment highlights the clinical need for improving outcomes of liver cancer.
Where a typical ultrasound uses sound waves to produce images of the body’s interior, U-M engineers have pioneered the use of those waves for treatment. And their technique works without the harmful side effects of current approaches such as radiation and chemotherapy.
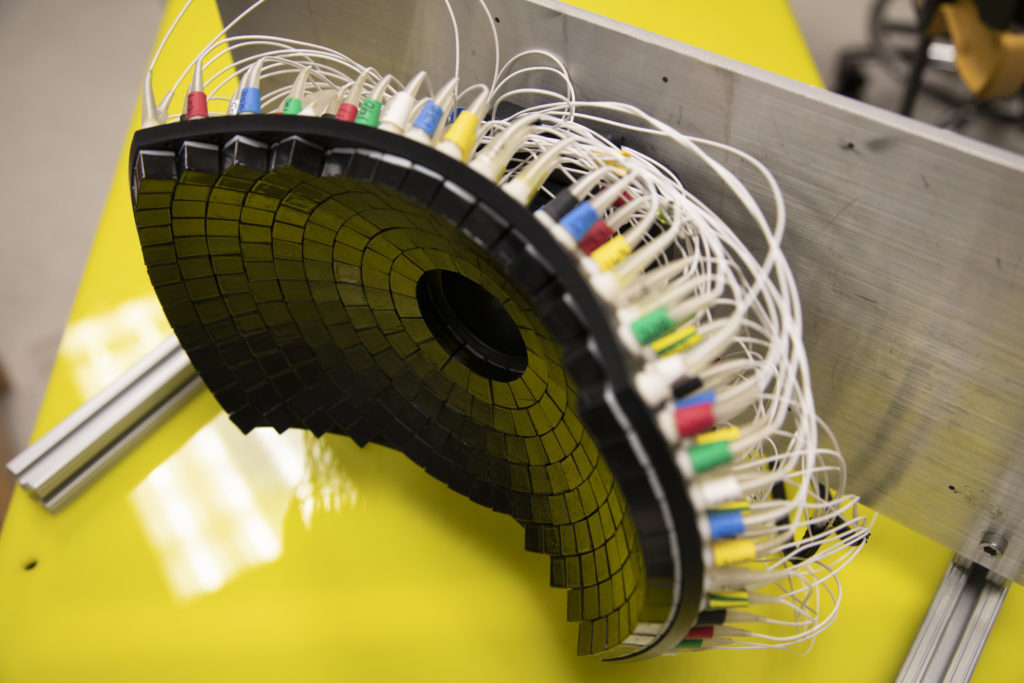
“Our transducer, designed and built at U-M, delivers high amplitude microsecond-length ultrasound pulses—acoustic cavitation—to focus on the tumor specifically to break it up,” said Xu. “Traditional ultrasound devices use lower amplitude pulses for imaging.”
The microsecond long pulses from UM’s transducer generate microbubbles within the targeted tissues—bubbles that rapidly expand and collapse. These violent but extremely localized mechanical stresses kill cancer cells and break up the tumor’s structure.
Since 2001, Xu’s laboratory at the University of Michigan has pioneered the use of histotripsy in the fight against cancer, leading to the clinical trial #HOPE4LIVER sponsored by HistoSonics, a U-M spinoff company. More recently, the group’s research has produced promising results on histotripsy treatment of brain therapy and immunotherapy.
The work represents a collaboration among engineering, medicine and public health. Xu and Timothy Hall, a research scientist in biomedical engineering, prepared the device that delivered the ultrasound waves. Worlikar, Man Zhang and Mishal Mendiratta-Lala, an assistant and associate professor of radiology, performed the histotripsy procedure on the rats. Worlikar, Clifford S. Cho, the C. Gardner Child Professor of Surgery, and Anutosh Ganguly, an assistant research scientist in surgery, measured and analyzed the tumor response and immune effects in the rats.
Jiaqi Shi, associate professor of pathology, analyzed histology data to evaluate tumor regression, recurrence or metastases. Lili Zhao, a research associate professor in biostatistics in public health, ran the analysis that showed the effectiveness of the approach. Fred Lee, a professor of radiology at the University of Wisconsin, assessed how relevant the results in rats are to humans. Mendiratta-Lala, Cho and Lee are involved in the current #HOPE4LIVER histotripsy clinical trial.
This study was supported by grants from the National Institutes of Health (NIH) (R01 CA211217 and K08 CA234222), the Focused Ultrasound Foundation, VA Merit Review 1I01BX001619-05, the University of Michigan Forbes Institute for Discovery, and the Michigan Medicine-Peking University Health Sciences Center Joint Institute for Translational and Clinical Research.
U-M retains a financial interest in HistoSonics, as do a number of researchers who were involved in this project and who helped develop the technology, including Xu, who is a company founder, stockholder and consultant. Each stands to benefit financially from the success of the platform.