Histotripsy: A potential approach to stroke treatment
The noninvasive technique uses focused ultrasound to create cavitational microbubbles that can break up tissue.
The noninvasive technique uses focused ultrasound to create cavitational microbubbles that can break up tissue.
Intracerebral hemorrhage, a life-altering type of hemorrhagic stroke, occurs in about 10 to 15 percent of all stroke cases. Individuals who suffer an ICH have a higher rate of disability and death – with about 60 percent of patients surviving at one month – than in other forms of stroke.
Once the bleeding stops following an ICH, a blood clot, or hematoma, forms. “These clots can range from marble-sized — just a few milliliters — to slightly smaller than a tennis ball,” says Tyler Gerhardson, a fourth-year doctoral candidate in the research group of BME Associate Professor Zhen Xu.
Gerhardson, Xu, and Jonathan Sukovich, an assistant research scientist also in BME, along with collaborators in the departments of Neurosurgery (Drs. Aditya Pandey and Neeraj Chaudhary) and Pathology (Dr. Sandra Camelo-Piragua), are working on a potential new treatment approach to breaking up those dangerous clots in the aftermath of an ICH. Their work was recently published in the journal Neurosurgery.

Conventional treatment of ICH has presented clinicians with several challenges. Since the clot increases pressure inside the skull as it grows, brain tissue is injured. Then, once the clot begins to break down in the days following the initial ICH, inflammatory and other processes release substances that are toxic to neighboring tissue, causing secondary injury.
Current treatment approaches include removal of the clot as early as possible and in a minimally-invasive way to avoid further damage and to prevent the vessels involved from bleeding again.
“There are a range of minimally-invasive methods to removing the clot, but they all have some limitations,” Gerhardson says.
The most recent clinical approach involves inserting a catheter into the clot through a small hole in the skull. Medication to dissolve the clot is given through the catheter, and the liquefied clot is drained the same way.
The procedure carries the risk of inducing rebleeding and is very slow, Gerhardson says, taking several days and still typically only removing about half of the clot. The long treatment time increases the risk of secondary brain damage.
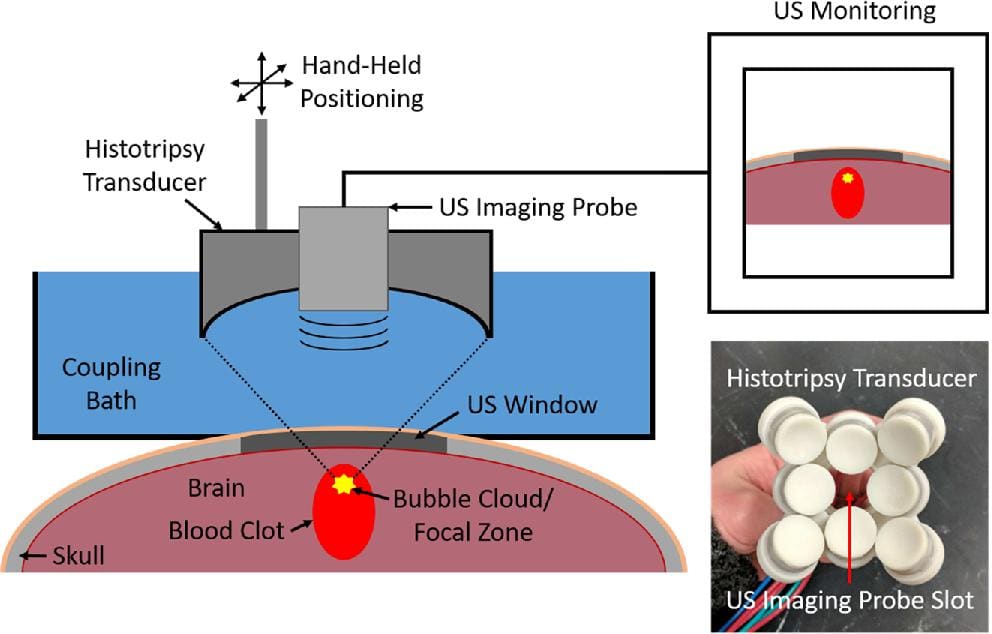
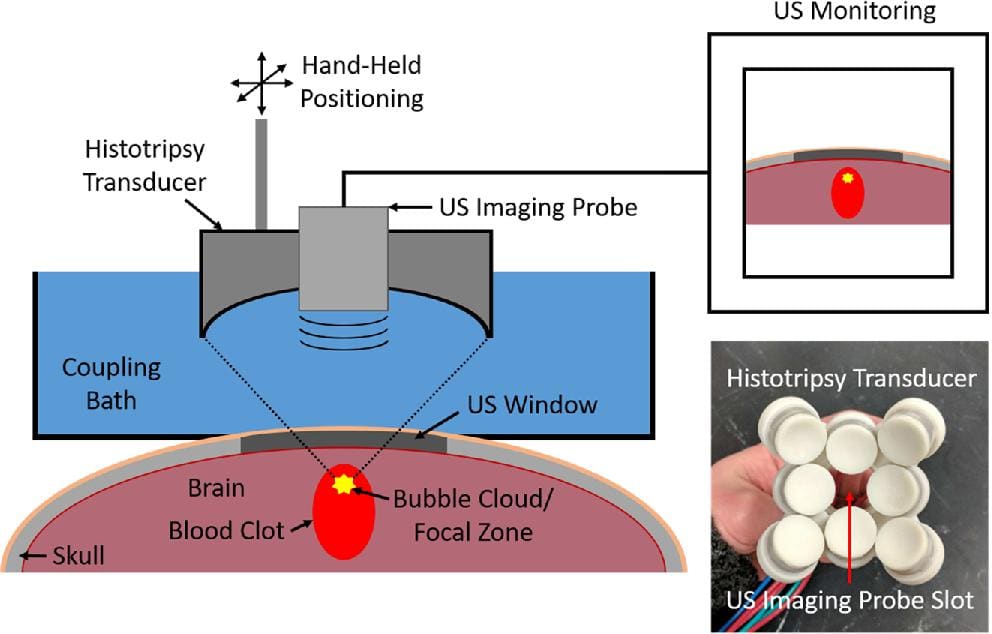
Now Gerhadson, Xu, and collaborators are investigating a new ultrasound-based technique, developed at U-M, to treat ICH. The noninvasive technique is known as histotripsy, and it uses focused ultrasound to create cavitational microbubbles that can break up tissue. Their work applying histotripsy to ICH was detailed in the article, “Histotripsy Clot Liquefaction in a Porcine Intracerebral Hemorrhage Model.”
Other research groups have used ultrasound to treat clots in different disease states, including deep vein thrombosis, or DVT, as well as smaller clots in ischemic stroke and large hematomas resulting from sports injuries, Gerhardson explains.
“But these techniques have relied on the administration of microbubbles or thrombolytic drugs to allow ultrasound to effectively liquefy the clots,” he says.
In contrast, histotripsy itself can generate microbubbles within the tissue. “Because of its purely mechanical mechanism of liquefaction, it’s well-suited to rapidly liquefy clots, without any injection of microbubbles or thrombolytic drugs,” Gerhardson adds.
“BECAUSE OF ITS PURELY MECHANICAL MECHANISM OF LIQUEFACTION, IT’S WELL-SUITED TO RAPIDLY LIQUEFY CLOTS, WITHOUT ANY INJECTION OF MICROBUBBLES OR THROMBOLYTIC DRUGS.”-Tyler Gerhardson
The goals of the recent study were two-fold: First, the research team set out to evaluate initial safety concerns, namely that rapidly liquefying the clot would cause the release of toxins that might injure nearby tissue and lead to poor functional outcomes or death.
Second, the group aimed to assess the ability to use a simple drainage technique — such as via catheter or a needle and syringe — to remove the histotripsy-treated liquefied clots.
Prior to this study, no group had investigated histotripsy use to liquefy clots in the brain in an in vivo model.
Overall, the U-M team found that it could use histotripsy to accurately target and liquefy the clots and easily drain them. No deaths, poor neurologic outcomes or additional tissue damage, beyond what was expected from the initial formation and presence of the clot, were observed, Gerhardson notes.
Although a number of questions that require further investigation remain, this study addresses initial concerns and represents a step toward translating the technology for use in ICH patients in a clinical setting — a tremendous unmet need.
“Clinicians need a minimally-invasive method to treat ICH that can be applied immediately and facilitate the clot’s removal within minutes,” Gerhardson says. “Histotripsy has the potential to achieve this. Translated to real ICH patients, it could significantly improve their survival and functional outcomes.”
The study was funded primarily by a National Institutes of Health an R21 grant (R21 NS093121).
Gerhardson T, Sukovich JR, Chaudhary N, Chenevert TL, Ives K, Hall TL, Camelo-Piragua S, Xu Z, Pandey AS. Histotripsy Clot Liquefaction in a Porcine Intracerebral Hemorrhage Model. Neurosurgery. 2019 Mar 29. pii: nyz089. doi: 10.1093/neuros/nyz089. [Epub ahead of print]